Samsung is seeking to venture into a new area for consumer health tech, according to people briefed on the company’s plans: putting sensors on a phone that can analyze air quality and sense things like temperature and humidity. Models trained on passively collected behavioral data — think typing cadence, app usage rhythms, sleep patterns, walking gait, call and messaging frequency, and even voice characteristics — were able to detect patterns that correlated with cognitive decline.
How a phone and watch record cognitive health signals
Contemporary smartphones and wearables produce a rich stream of “digital biomarkers.” Based on those, the researchers at Samsung concentrated on a few particularly revealing signals. Keyboard dynamics — such as how long people pause between keys or before difficult words, and how often they backspace or rely on autocorrect — can reflect processing speed and executive function on phones. On wrist-worn devices, inertial sensors record other gait characteristics such as stride time variability, turn speed, and pace symmetry that are found to alter as cognitive decline progresses.
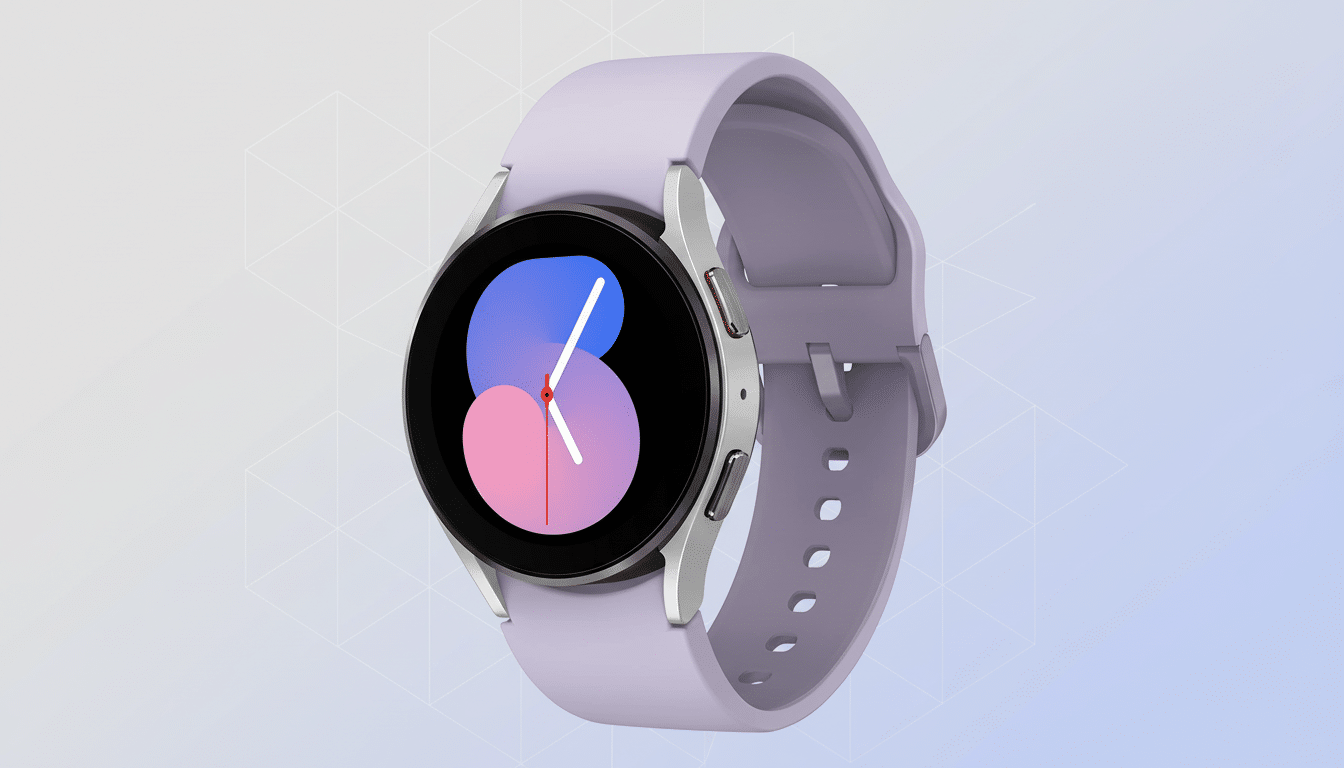
Two pilot studies were particularly notable, the company said: one that looked at typing patterns and another that combined motion data from the phone and Galaxy Watch to measure walking. Preliminary results indicated performance in line with standard clinic-based screening tools for memory care and, as such, are a significant result — all the more so given that these models were trained on ambient, rather than structured test data.
The approach also piggybacks on sleep and voice. Fragmented sleep and a lower proportion of REM have been associated in academic studies with risk for cognitive impairment, while voice analytics — such as pauses, articulation rate, and prosody — can pick up on subtle linguistic changes. It’s not the diagnosis per se from any one signal; it is a mosaic of many weak signals adding up to a stronger, more individually personalized risk profile.
Why early detection of cognitive decline truly matters
Alzheimer’s disease takes hold years before symptoms appear obvious. The Alzheimer’s Association calculates that millions of older adults in the United States have Alzheimer’s dementia, and the World Health Organization estimates global prevalence to be tens of millions. If cognitive changes can be caught earlier, it can allow clinicians to confirm causes, manage reversible contributors, plan care, and think about treatments or trials when they are most likely to help.
Conventional screening is based on sporadic medical visits and paper-and-pencil tests. Passive sensing provides a complementary avenue: measuring continuously in everyday life. That longitudinal view can help separate normal variability from persistent decline and may detect changes long before family members or co-workers notice.
What this would look like on Galaxy devices
If Samsung does bring it to consumers, I sure hope we get an opt-in experience; clear consent flows and a reiteration that the company — like Google with most Assistant features — must prioritize on-device processing for privacy concerns. One realistic design might be to perform local computation of models, summarize trends periodically, and only surface a notification if sustained changes exceed an “important” threshold. Instead of giving a diagnosis, it’d probably encourage the user to take a validated cognitive screener test or discuss the result with a clinician.

Data privacy and sovereignty will be central. Health data is one of the most sensitive categories a device can track, and users will expect granular settings, clear explanations, and the ability to stop or delete collected signals. Collaborating with academic institutions and health systems could also help to see that the resulting guidance lands within clinical workflows.
Accuracy, bias, and regulatory barriers
Transitioning from a promising experiment to a reliable feature takes diverse, large-scale validation. Typing and speech differ by language; walking patterns vary as we age and move through different cultures or environments; phone habits shift with jobs or caregivers in our lives. Models will have to be stress-tested to avoid bias, and calibrated so as not to generate false alarms that might cause anxiety — or false reassurance that could delay care.
Any device that purports to estimate disease risk slides into regulated territory. In a number of jurisdictions, software that processes physiological or behavioral data in a health context can be regulated as if it is a medical device and so would need to meet stringent evidence standards, post-market monitoring, and have well-defined software labeling. Expect a phased rollout: research apps first, then limited features presented as wellness insights, and only after considerable evidence of reliable quality, clinical-grade capabilities.
Part of a bigger wave in digital biomarker research
Samsung’s efforts fall in line with a broader push toward sensor-based health intelligence. Wearables have already proven that they can flag irregular heart rhythms, and research programs have delved into the Parkinson’s tremor; changes in speech caused by neurodegenerative disease; and sleep metrics linked to mental health. Nonprofits and research consortia are funding digital measures that can speed trials by finding change sooner — and more objectively than subjective scales.
The bottom line on Samsung’s cognitive monitoring plans
The company’s phone-and-watch strategy for cognitive monitoring is still a work in progress, but the idea is tantalizing: unobtrusive sensors that reveal early, actionable signals. If the company can prove both accuracy at scale and privacy protections to gain clinical trust, Galaxy devices might graduate from fitness companions to tools that help people know when something deeper might be changing — and reach out for help sooner.

