Can artificial intelligence really help radiologists find breast cancer sooner — or does it risk ensuring they don’t find that which we aren’t looking for? A one-of-a-kind $16 million randomized trial involving 7 U.S. medical centers seeks to provide some of the hard answers by gauging how much (if any) AI help enhances screening mammography in a practical, real-world setting.
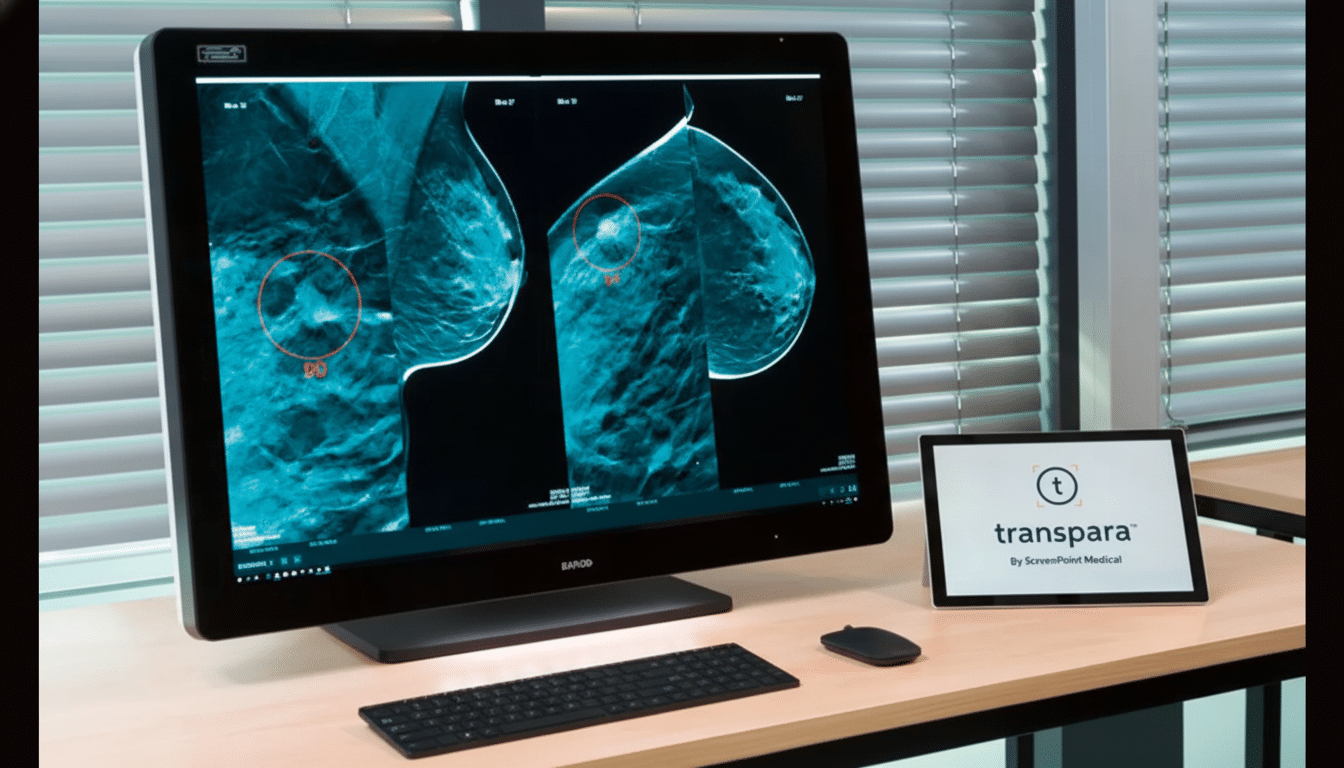
The PRISM (Pragmatic Randomized Trial of Artificial Intelligence for Screening Mammography) study will pit standard radiologist reads against Transpara-aided reads, powered by ScreenPoint Medical’s FDA-cleared decision support system. Every test still has a human final judgment; the question is whether AI nudges performance up or down when the stakes are highest.
Why This Trial Matters for Breast Cancer Screening Now
Breast cancer is still the most diagnosed cancer in U.S. women, and early detection is strongly associated with better outcomes. Mammography saves lives, but it has blind spots. The sensitivity is known to vary with breast density and age, and the burden of false alarms goes far beyond inconvenience — studies estimate that over a decade of annual screenings, more than half of women will have at least one false-positive callback, which brings extra imaging, biopsies, costs and stress.
The other side of this problem is missed cancers and interval cancers (cancers that are detected between screenings). Dense tissue — which can be found in about 40 percent of women — obscures subtle findings, and small lesions or architectural distortions are easy to miss in a busy clinic. Meanwhile, if AI can cut unnecessary recalls and catch more clinically significant cancers, that would be a double bonus — gains like this are rare.
There’s also more recent history to take into account. Previous generations of computer-aided detection were embraced — but later found to raise false alarms without enhancing outcomes. Modern deep-learning systems are much more sophisticated, but policymakers, clinicians and patients all seek evidence that translates beyond curated test sets.
How the PRISM Trial Operates Across Seven U.S. Centers
PRISM, led by UCLA and UC Davis and including Boston Medical Center, UC San Diego Health, University of Miami, the University of Washington–Fred Hutchinson Cancer Center and the University of Wisconsin–Madison, will randomize hundreds of thousands of screening exams to two groups: radiologist alone versus radiologist read with AI decision support.
Key metrics include cancer detection rate, recall rate, biopsy positive predictive value and interval cancer rate — measures of both sensitivity and specificity, not simply headline accuracy. The trial also incorporates surveys and focus groups to understand how patients and health care providers perceive and trust care that is assisted by AI, which is a key ingredient for the successful adoption of these services.
With a pragmatic, multicenter design, it is suggested that results from some centers represent what would be expected in daily clinical practice despite different populations, types of scanners and workflow patterns — scenarios where AI tools often fail due to variability of data and devices.
What We Know From Other Studies and Trials So Far
Retrospective studies have been encouraging. A much-cited analysis from Google researchers claimed lower rates of both false positives and false negatives compared with the average radiologist on large data sets. In Europe, prospective analyses have suggested efficiency gains, with a Swedish population-based study finding so-called AI-supported single reading would reduce workload by approximately 40% without compromising cancer detection compared with traditional double reading.
But retrospective and observational results can fail in routine practice, and the benefits aren’t equal across vendors or sites. One Harvard-affiliated academic study that came out recently raised automation bias as a potential concern — clinicians may become too dependent on AI suggestions, especially when under time pressure. That’s precisely why randomized, real-world trials like PRISM are so important: they test whether those performance lifts survive when you stress the system with patient heterogeneity, equipment variation, and workflow constraints.
Another open question is modality mix. Much of the United States now uses digital breast tomosynthesis (3D mammography), which enhances detection in dense breasts. The added value of AI to tomosynthesis could be different from its added value with conventional 2D mammography. A subgroup analysis of PRISM on age, breast density, and modality should be possible due to its large sample size.
The Stakes For Patients & Health Systems
Positive results could radiate out from the reading room. If AI leads to lower recall rates without increasing interval cancers, insurers could see fewer downstream costs tied to excess imaging and procedures. Health systems could help relieve workforce pressure on thousands of aging radiologists who are preparing to retire, and take on screening volumes. And patients may no longer have to endure so many sleepless nights waiting for repeat scans.
But benefits must be equitable. When skewed datasets are used to train AI, this can result in underperformance in underrepresented groups. External validation in various populations — and post-deployment audits over time — will be essential. Regulators are already supposed to ask manufacturers about performance drift as software updates and imaging hardware change.
Importantly, not all “upgrades” are treated the same. A pure spike in sensitivity (which primarily adds indolent lesions) could drive overdiagnosis; the most persuasive signal would be a decrease in interval and advanced-stage cancers, while holding recalls at bay. That’s the clinical needle PRISM is designed to thread.
What to Watch Next as PRISM Reports Early Results
Three outcomes will define success:
- That AI-assisted reads make clinically significant cancers easier to find.
- That recall and biopsy rates decrease or at least do not increase.
- That benefits are consistent across subgroups, specifically women with dense breasts and across imaging platforms.
If the balance pushes positive, expect to see movement at warp speed on reimbursement, procurement and quality measures. If the results are mixed, health systems could choose to use them selectively — triaging low-risk exams or second looks in dense breast cases. In either case, PRISM may replace hype and doubt with evidence, rendering not just where AI fits for breast cancer screening but also when the human eye should still lead.

