What if a breath into a cartridge followed by a few minutes of canine sniffing could flag cancer at its earliest stages and help prevent untold deaths?
SpotitEarly, an Israeli-founded startup, is pairing dogs with machine-learning analytics to form a non-invasive, multi-cancer screening that aspires to be accurate and widely available for real-world clinics.
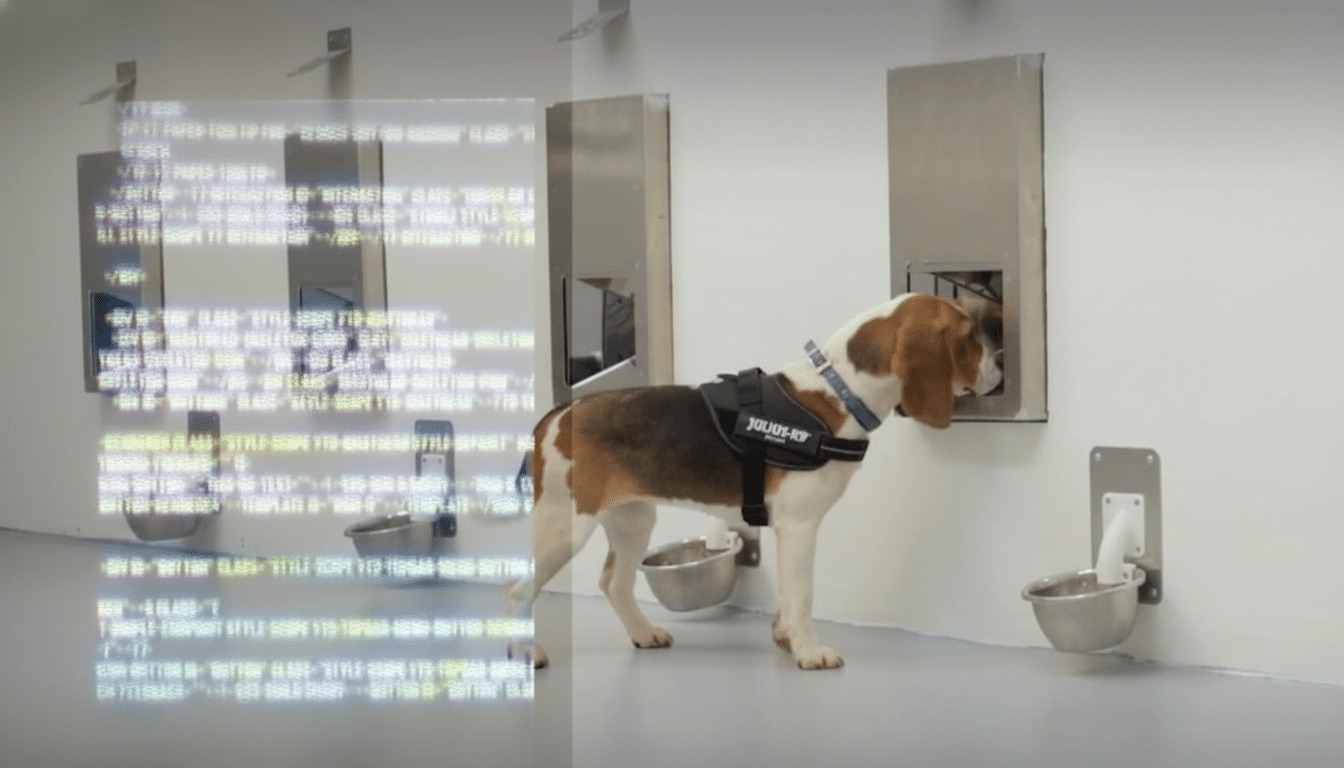
The company’s method revolves around at-home breath collection kits that are mailed to a central laboratory, where they are screened by a pack of professionally trained beagles for certain volatile organic compounds associated with cancer.
A layer of AI tracks each dog’s behavior and physiology in real time, standardizing the readouts and minimizing human bias.
How SpotitEarly’s breath test and canine-AI screening works
Cancers reprogram metabolism and release unique volatile molecules that show up in breath. Dogs can sniff these trace signatures, which appear from minute particles as early warning signs of the disease, when they are still far too minimal for most instruments. SpotitEarly collects exhaled substances on a disposable cartridge, loads it into the system, and presents the sample to its canine team in controlled conditions.
Cameras monitor posture and stillness above each lane, microphones record breathing cadence, and sensors track heart rate. The company’s model is trained on each dog’s baseline and raises a flag for deviations that carry implications of “cancer positive.” By demanding agreement among several dogs and quantifying behavior in standardized units, as opposed to being interpreted by a handler, the system is meant to enhance reproducibility.
This hybrid approach draws lessons from effective public safety and health detection-dog programs — think explosives detection or hypoglycemia alerts among diabetics — but with quantification and audit trails that have been absent from traditional canine assays. It’s an ancient sense, overhauled for modern diagnostics.
What the early data suggests about SpotitEarly’s accuracy
In a published double-blind clinical study in Scientific Reports, a Nature Research journal, SpotitEarly claimed 94% accuracy overall with screening of breath samples from approximately 1,400 patients. The work concentrated on four of the most prevalent cancers — breast, colorectal, prostate, and lung — with early detection taking precedence.
Accuracy is a mix of sensitivity and specificity, which matter for screening. Independent replication and larger, multi-center cohorts will be necessary to confirm stage-by-stage performance, rule out confounders such as smoking or diet, and cement real-world false-positive rates. Like other multi-cancer early detection tests, regulatory clearance lies ahead; for now most offerings are run in physician-ordered certified labs as more evidence is collected.

The promise is significant. Early detection leads to much better outcomes, as the American Cancer Society and National Cancer Institute point out — controlled or localized breast and prostate cancers have excellent five-year survival rates; colorectal cancer’s surpasses 90% when caught early; for lung cancer, the five-year survival rate jumps from about 8% in advanced stages to around 60% or more when it hasn’t spread.
Pricing and the broader landscape of multi-cancer early detection
Breath-based screening joins an expanding multi-cancer early detection (MCED) space. These days, consumers can have a doctor order blood-based screens such as Grail’s Galleri test or use services offering whole-body MRIs from outfits like Prenuvo and Ezra. Courts are entering orders permitting MCED testing pending while FDA approval is being developed.
SpotitEarly says it plans to price a single-cancer breath test at around $250, with incremental add-ons for other cancers coming in below that amount, and any multi-cancer panel below the price of leading blood tests. The company expects to route the kits through a network of physicians, offering confirmatory paths for positives and guidance on follow-up imaging or diagnostics, because that’s essential if patients are not to be subjected to unnecessary treatments.
Inside the canine training program powering the breath test
The startup currently employs 18 beagles, known for their olfactory abilities and genetics that produce orange coats and an even temper. Training is through positive reinforcement associating target odors with a sit-and-stay alert, and regular “blank” and control runs prevent cueing and overfitting. There are multiple dogs per sample, and the AI is comparing responses with historical pack performance to dampen outliers and fatigue effects.
There is some precedent for canine detection: detectors in the UK, along with academic groups from the University of Pennsylvania, have shown that dogs can detect odors associated with diseases with very high sensitivity under controlled settings. What SpotitEarly contributes is a way of turning that capacity into a standardized process in the lab with machine-measured endpoints, which clinicians need to scale up for patients.
Road map, upcoming trials, and what to watch for next
Funded with $20.3 million from investors including Hanaco VC, Menomedin VC, Jeff Swartz, and Avishai Abrahami, the company is expanding into U.S. trials starting with breast cancer before rolling out more studies in colorectal, prostate, and lung cancers. Key priorities include larger and more varied cohorts, head-to-head comparisons with other accepted screening modalities, and rigorous quality controls in a CLIA laboratory setting.
Two big questions loom. The first is scalability: if they’re trained on dogs, that’s obviously a niche, so the AI layer should be able, in principle, to steer an electronic-nose system (that mirrors the dogs’ detection patterns) down a path now being explored throughout breathomics by companies like Owlstone Medical. Second, clinical integration: a positive breath screen must be value-added and fit easily into guidelines-driven care; lead to appropriate follow-up testing and treatments; and reduce diagnostic odysseys.
If the findings hold up, a low-cost breath test that screens for an array of cancers might help widen access to lifesaving early detection. One approach that might lead to such a transformative test is to combine nature’s best biosensor with modern AI — an unusually pragmatic route, if it pans out.

