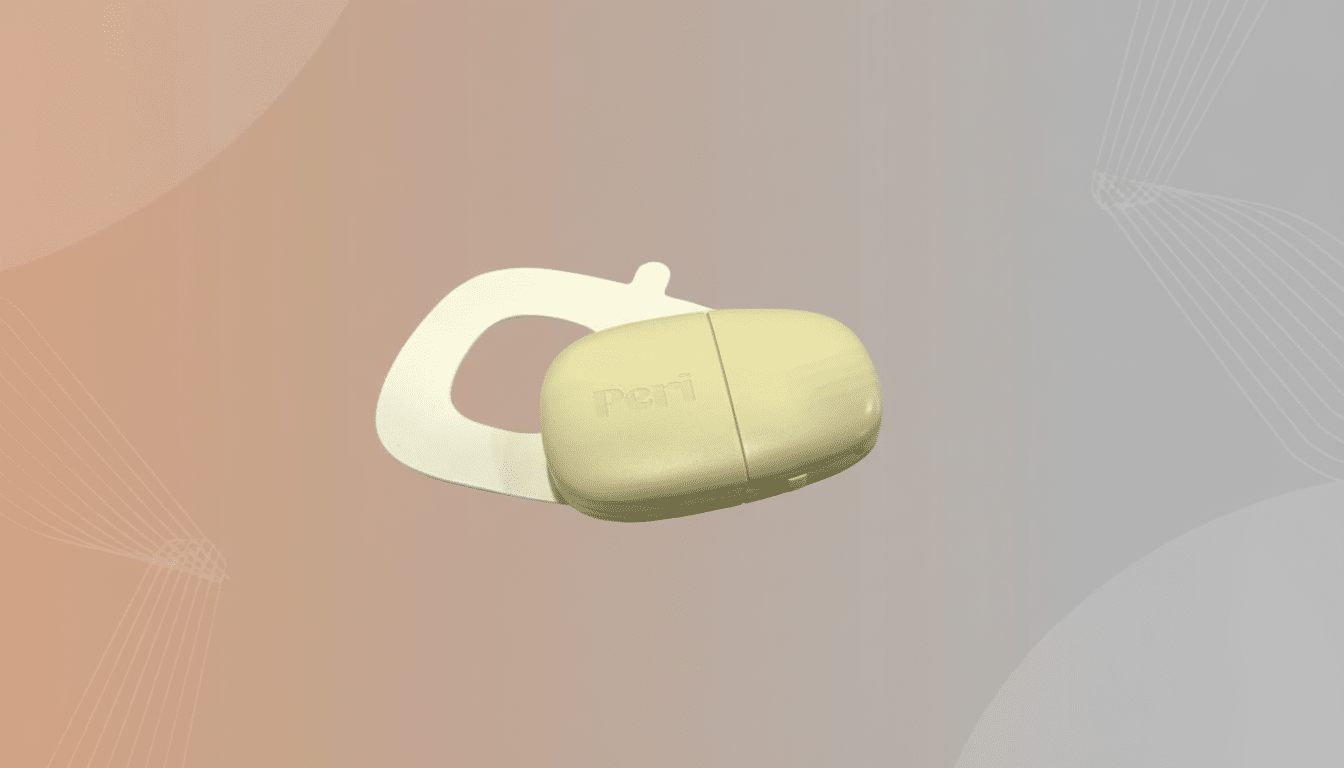
I arrived into the health halls, expecting another wristband or smart ring to dominate. Instead, the most influential women’s health tracker on the floor was a neat little adhesive patch made specifically for perimenopause. One such device is Peri, created by IdentifyHer, which isn’t trying to be all things for everyone — it’s zeroing in on the messy, misunderstood period leading up to menopause. And that clarity of purpose is what stands out.
What Sets Peri Apart in Perimenopause Tracking
Peri fits like a noninvasive continuous glucose monitor, resting below the breast where it can read small changes in the body. The $449 device marries four sensors — PPG for blood flow, an accelerometer for motion, an EDA sensor for skin conductance, and a temperature sensor — with an on-device algorithm tuned to detect the patterns of someone who is perimenopausal. It gets about seven to 10 days between charges, before snapping off, recharging, and applying again.
But rather than red-flag a hot flash just by temperature, Peri crosshatches several signals to pick up the telltale vasomotor waterfall, differentiating it from exercise, stress, or ambient heat. Sleep timing, anxiety scoring, activity level, and cycle info are all surfaced in a clean home screen, plus the app has a journaling tool to capture mood and symptoms. Users can also add labels for hormone therapy and track how interventions correspond to sleep, hot flashes, and daytime function over time.
Designed for Perimenopause, Not Just Periods
Perimenopause is not a niche: According to the North American Menopause Society, it frequently lasts four to eight years and includes fluctuating estrogen levels, irregular cycles, hot flashes, night sweats, disrupted sleep, brain fog, and mood changes. NAMS also points out that vasomotor symptoms affect the majority of women, with a large percentage having moderate to severe ones. By 2030, the organization estimates that there will be approximately 1.2 billion menopausal women globally, with tens of millions entering the transition each year.
Many generalist wearables simply bolt on period or fertility features to broad readouts like wrist temperature or resting heart rate. That’s valuable, but it may miss out on the midlife picture. Peri flips the model: Instead of placing sleep, stress, and activity at its center, it puts perimenopause there, then layers up from that lens with the other elements. The goal, according to Heidi Davis, IdentifyHer’s CEO, is to bring women out of “powering through” and into a world where the empirical data exists to support what they feel and unambiguously guide next steps. Replacing fuzzy self-reporting with more reliable biometrics to track symptoms can create a more consistent and actionable way of tracking, says COO Donal O’Gorman.
Clinical Implications and the Menopause Knowledge Gap
There’s a well-documented gap in care here. Studies published by menopause specialists have found that fewer than 1 in 5 OB‑GYN residents are confident in their ability to provide comprehensive care for menopausal patients, and many providers have not received formal training on this phase. Quantitative measures might help move the conversation from “I feel like I’m having more hot flashes” to “I had clustered, EDA‑confirmed episodes between 2 a.m. and 4 a.m. three nights this week,” clearer evidence for how to adjust therapies.

Peri’s approach isn’t just a variation on other models of this process: Studies have used skin conductance to record hot flashes for decades, looking at how well these readings track with self-reported events and capturing nighttime episodes that people don’t remember having. Factor in changing temperature and the tossing and turning, and you can begin to tease apart whether night sweats are associated with changes in sleep stage — or evening alcohol or late workouts.
How Peri Compares With Today’s Popular Wearables
Other cycle-tracking rings and watches from well-known brands are also more advanced than a period app, with the capacity, in some cases, to predict ovulation windows based on temperature trends. Few have EDA for stress, though; hot‑flash detection is rarely a first‑class feature, and insights about perimenopause are often hidden. Peri’s chest form factor and multimodal signal set are designed for vasomotor events and sleep disruptions — specifically the problems that define this life stage, as opposed to trying to wedge a fitness device into a medical‑adjacent use case.
Peri was also acknowledged as an honoree for a CES Innovation Award, in the category of digital health — which suggests that its category definition and hardware selections are a hit with judges looking at meaningful, high‑impact design rather than another step‑counting device.
Early Caveats to Watch Before Buying or Using Peri
Peri costs $449, putting it in the same category as many high-quality wearables; its value will be determined by how well it measures up for accuracy, comfort, and the caliber of insights it delivers. Adhesive comfort across skin types, sensor performance across a wide range of body compositions, and transparency in privacy practices will all matter. Potential buyers should seek peer‑reviewed validation data and clarifications on whether Peri is being marketed as a wellness device or following regulatory pathways. Battery life of up to 10 days is good, but reapplying it a lot could be one thing that wears on some people.
The Bottom Line: Why Peri’s Focus Could Matter Most
At a time when trackers abound that promise marginal gains by tracking steps or recovery scores, Peri gets top billing because it is directed at the women who are most underserved by mainstream wearables. It channels a tumultuous, yearslong transition into something concrete and actionable for people to use — on their own or in tandem with clinicians. Was the most memorable women’s health innovation at CES really a perimenopause patch? No, it wasn’t, but that’s precisely why it matters: It addresses the largest gap with a tool that fits.

