Oura unveils a revamped app with Cumulative Stress. Oura is releasing a redesigned app experience that focuses on a new Cumulative Stress metric based on its smart ring that now offers more than rest and recovery, addressing how a person’s body responds to lasting strain. The refresh includes more transparent navigation, more expansive long-term perspectives, and a study-crafted foray into blood pressure risk assessment, for which the firm intends to seek U.S. regulatory authorization.
Unlike the stress score at the moment, the past month’s data and weekly updates on Oura’s Cumulative Stress indicate how strain accumulates or vanishes. The metric combines five factors, which frequently adjust with chronic load:
- Sleep continuity
- Heart stress response
- Sleep micro-movements
- Temperature regulation
- Activity impact
In reality, that implies the Cumulative Stress score will be increased by disturbed sleep, raised cardiovascular strain, or a restless micro-movement pattern, while steady sleep and well-timed activity levels might reduce it. That long-view strategy is consistent with the advice of many physiologists; continuous stress is not gradual but, rather, a persistent signal over several weeks. Studies summarized by the American Heart Association have linked continual stress with elevated blood pressure and reduced heart rate variability, while a cohort study has revealed a disrupted sleep pattern linked to a higher cardiometabolic risk profile. By amalgamating various physiological ideas, Oura is convinced that it can assist users in noticing the trend before it turns into a problem.
For instance, a marathon trainee who is piling up intense workouts plus travel and late nights might see increasing Cumulative Stress even if daily workout readiness appears respectable. A week of going to bed earlier and more gently could also temper the pattern, with a starker feedback loop than single-day readouts.
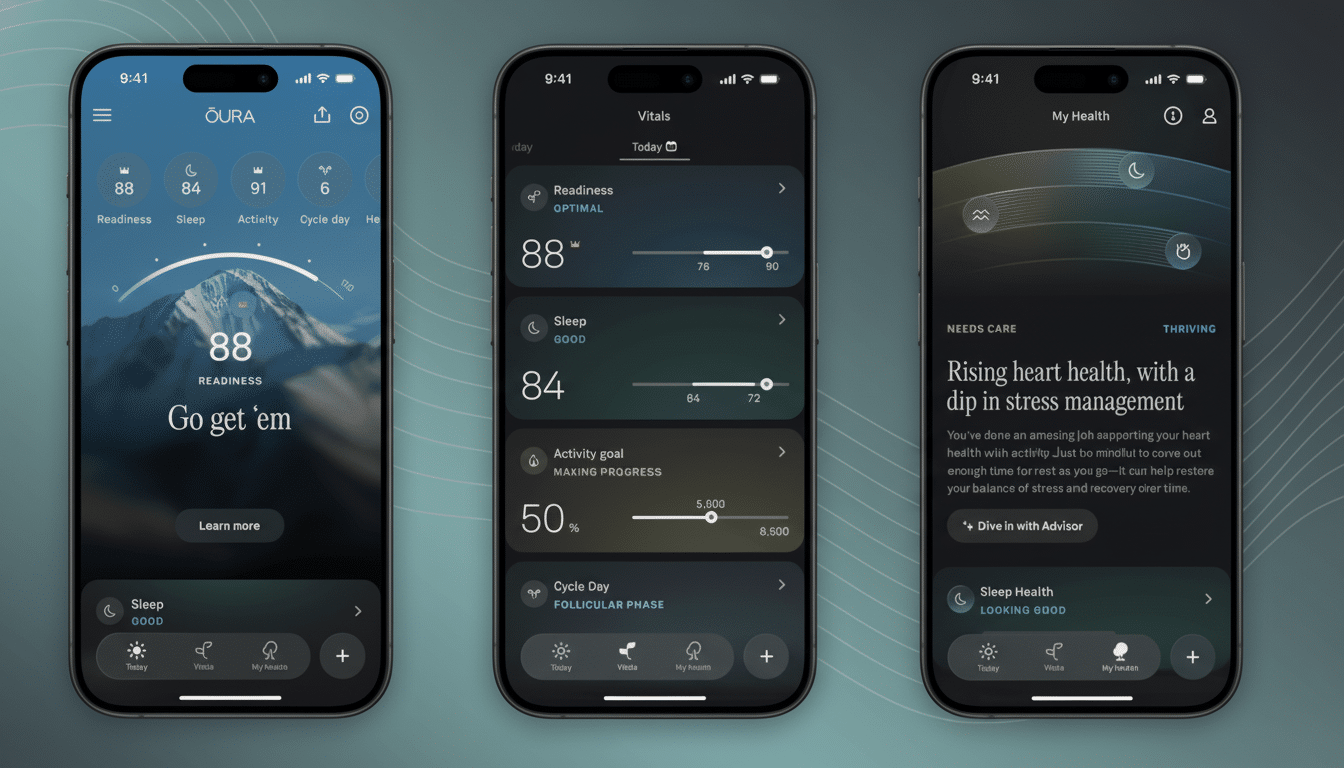
Inside the redesigned Oura app: tabs, trends, and cycles
It now has three tabs in the interface, and it splashes right at you. Today brings up the most relevant insights for what I can do immediately, like whether to scale back training or place an emphasis on wind-down habits. Vitals gives you a quick view of sleep, stress, and cardiovascular trends, so it’s less cumbersome to look for inflections without having to dive into menus. My Health focuses on longer-term trends and includes Habits and Routines, which let you get credit for regular actions such as being exposed to morning light, eating dinner earlier, or having late caffeine.
Cycle insights get a boost here, too. The app also broadens from a one-month to a 12-month view of period and fertile window forecasts — an upgrade that appears likely to be useful for people who schedule training cycles, travel, or otherwise plan around anticipated shifts. More time can help make such surprises less likely and offer a clearer, stable line to negotiate with doctors if patterns do change.
Moving toward cuffless blood pressure guidance and FDA review
As part of the redesign, Oura is seeking clearance from the U.S. Food and Drug Administration for functions that estimate a user’s probability of hypertension as well as other health issues. And as one part of that pathway, the company is launching a U.S.-based IRB-approved Blood Pressure Profile study in its Oura Labs program to gather ring-derived signals alongside a simple check-in about family history, medications, and lifestyle. Participants will be given a none, mild, or severe indication of hypertension and encouraged to seek help from a clinician as appropriate.

At present, the regulatory bar for cuffless blood pressure is high. Clinical-grade wearables, such as an inflatable-cuff watch, have FDA clearance, but most optical and model-based methods remain investigational in the U.S. Other consumer devices, including some smartwatches, provide blood pressure features in some localities but need to be calibrated often and have yet to be cleared for domestic diagnosis. Oura’s framing — a probability inference and serial monitoring, rather than a one-off blood pressure measure — points toward a stepwise pathway that fits the current FDA expectations.
The public health setting is important. High blood pressure afflicts nearly half of all American adults, the Centers for Disease Control and Prevention have estimated, but only about one in four has it under control. Worldwide, the World Health Organization estimates some 1.28 billion adults are affected, most of them undiagnosed. Passive signals that raise a flag of heightened risk between clinic visits could help close that gap if they are effective and fair across diverse populations.
How Oura’s approach stacks up against competing wearables
Wearables, for their part, have really been driving toward stress analytics. Garmin measures stress based on heart rate variability and respiration; Fitbit’s “Stress Management Score” combines biometric indicators with mood check-ins; Whoop calculates daily strain and recovery. Oura’s differentiator is that it focuses on a weekly trend direction and has a multi-sensor composite optimized for chronic load (not spot reaction timing). If done well, that could reduce the alert fatigue of spiky, day-to-day scores and render the data more actionable.
The company has also been on a product cadence that would support deeper health use cases, like its Ring 4 Ceramic collection, first charging case, and Health Panels that let members schedule bloodwork directly in the app. An asset manager–led fundraise also underscores investors’ faith in wearables that transition from wellness to preventive health, a thesis that the Kinsa product supports.
What users should watch as Cumulative Stress rolls out
Motivation for most will stem from trend and behavior metrics in Cumulative Stress. If the score ticks upward for weeks on end, then think of concrete changes: going to bed earlier, taking a rest day somewhere in between bouts of high-intensity workouts, or “time-buffering” work and sleep with non-work-related time. On top of that, combining the metric with Routines allows users to try and establish what really makes a difference for them, instead of basing it on force-fed advice.
As with many things, stress and blood pressure are a hodgepodge. Wearable observations should supplement, not supersede, clinical measurements. But if Oura’s new instruments make more people catch early sustained overload and nudge them to seek timely care when hypertension risk emerges, that redesign will be about more than paint.

